Probiotics, the gut microbiome and feeding issues
Overview
The Gastrointestinal tract (GIT) is home to trillions of microbes, collectively called the gut microbiome. Extensive research shows that having the correct balance of good microbes is essential for our health. One way we can alter the balance of microbes in our gastrointestinal tract is through Probiotics. Probiotics are ‘live microorganisms that confer a health benefit’1. Probiotics are recognised as good bacteria that are found in food or food supplements. Research indicates that probiotics are safe and well tolerated in normal, healthy babies, children and adults.
Strain specific effects of probiotics
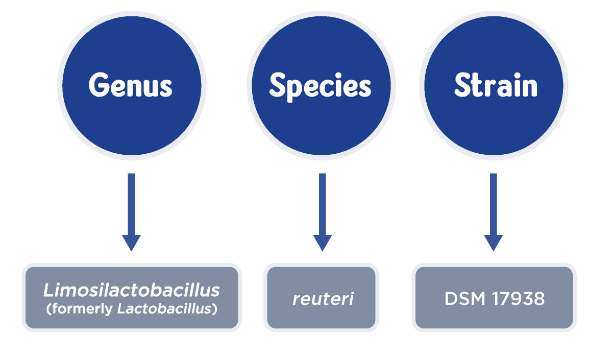
Probiotics are made up of bacteria, which can be classified into genus, species and strains. Within each species of bacteria there are a multitude of strains. Strains of bacteria within the same species can have significantly different modes of action, properties and characteristics and these are known as strain-specific qualities. Some strains within a given species are strong and resilient, with a demonstrated capacity to survive the trip through the upper GIT, interact with the immune system, and inhibit pathogenic bacteria, (e.g. L. reuteri DSM17938)2, whereas other strains are weak and cannot even survive transit through the stomach or small intestine. Therefore, it is important to remember that just because a probiotic strain works in one condition, it will not necessarily be effective for other conditions. For this reason, probiotic bacteria must be defined and tested in clinical trials at a strain level.
Infant gut health: the importance of a balanced microbiome
Infants are born with an immature immune system, and therefore need a balanced gut microbiome for their immune function and development2. Good infant gut health with a balanced microbiome is established during and post-birth, and changes over time in response to the infant’s external environment and nutrition. Nutritional strategies such as breastfeeding are crucial in the development of the gut microbiome as breast milk contains many microbes that colonise the infant’s gut2-4. Alterations in the gut microbiome have been strongly linked with common Functional Gastrointestinal Disorders (FGIDs) that present in the first year of life5.
Probiotics and Functional Gastrointestinal Disorders (FGIDs)
The cause of functional gastrointestinal disorder (FGID) in infancy is multifactorial but one of the most common denominators is the alteration in the bacterial microbiota. Research shows that an altered gut microbiota may play a key role in the development of infantile colic6. Clinical studies have shown that babies with colic have lower counts of good bacteria as well as increased number of harmful bacteria in their digestive tract and greater levels of inflammation7. In these babies, a particular strain of a probiotic known as L.reuteri DSM17938 has been shown to help reduce crying time especially in breastfed babies8,9. L.reuteri DSM17938 works by activating anti-inflammatory pathways, therefore reducing overall inflammation in the intestine10,11.
Find out more
View this webinar on demand to learn more about Probiotics for functional gastrointestinal disorders (nestlenutrition-institute.org)
This article was written by Registered Dietitian, Rachel Kumar (Medical & Scientific Affairs Manager for SMA Nutrition)
-
FAO/WHO. Evaluation of health and nutritional properties of powder milk and live lactic acid bacteria. Report from FAO/WHO Expert Consultation. 2001:1-4.
-
Mu Q, et al. Front Microbiol. 2018;9:757. Published 2018 Apr 19. doi:10.3389/fmicb.2018.00757
-
Moore RE, Townsend SD. Open boil. 2019;9(9):190128
-
Turroni et al. Ital J Pediatr, 2020;46(1):16
-
Vighi G et al. Clin Exp Immunol. 2008;153 Suppl 1(Suppl 1):3-6
-
Shamir et al. Journal of Pediatric Gastroenterology and Nutrition: December 2013 - Volume 57 - Issue - p S1. doi: 10.1097/MPG.0b013e3182a154ff
-
Savino F, et al. Acta Paediatrica. 2017 Apr;106(4):573-8.
-
Gutiérrez-Castrellón P, et al. Indrio F, Bolio-Galvis A, Jiménez-Gutiérrez C, Jimenez-Escobar I, López-Velázquez G. Efficacy of Lactobacillus reuteri DSM 17938 for infantile colic: Systematic review with network meta-analysis. Medicine. 2017 Dec;96(51).
-
Sung V, D'Amico F, Cabana MD, Chau K, Koren G, Savino F, Szajewska H, Deshpande G, Dupont C, Indrio F, Mentula S, Partty A, Tancredi D. Lactobacillus reuteri to Treat Infant Colic: A Meta-analysis. Pediatrics. 2018 Jan;141(1):e20171811.
-
Garcia Rodenas CL, et al. J Pediatr Gastroenterol Nutr. 2016;63(6):681-687
-
Liu Y et al. Am J Physiol Gastrointest Liver Physiol. 2010;299(5):G1087-G1096
IMPORTANT NOTICE:
The World Health Organisation (WHO) has recommended that pregnant women and new mothers be informed on the benefits and superiority of breastfeeding – in particular the fact that it provides the best nutrition and protection from illness for babies. Mothers should be given guidance on the preparation for, and maintenance of, lactation, with special emphasis on the importance of a well-balanced diet both during pregnancy and after delivery. Unnecessary introduction of partial bottle-feeding or other foods and drinks should be discouraged since it will have a negative effect on breastfeeding. Similarly, mothers should be warned of the difficulty of reversing a decision not to breastfeed. Before advising a mother to use an infant formula, she should be advised of the social and financial implications of her decision: for example, if a baby is exclusively bottle-fed, more than one can (400 g) per week will be needed, so the family circumstances and costs should be kept in mind. Mothers should be reminded that breast milk is not only the best, but also the most economical food for babies. If a decision to use an infant formula is taken, it is important to give instructions on correct preparation methods, emphasising that unboiled water, unsterilised bottles or incorrect dilution can all lead to illness.